This section is currently under revision/maintenance. Check back soon for the updated page.Sorry for the inconvenience!

Resources
Check below for FAQs/Resources you may find helpful!
Frequently Asked Questions
What is EMDR?
Eye Movement Sesensitization and Reprocessing (EMDR) was developed by Francine Shapiro (2001) initially for the treatment of PTSD. It is a therapeutic approach that involves bilateral stimulation of the client through alternating sensations (ie. Eye movements, tapping) while simultaneously focusing on a target memory to achieve a reduction in the vividness and emotional response. This interaction serves to stimulates communication between parts of the brain (amygdala, hippocampus, and prefrontal cortex) to manage and resolve traumatic responses. Then, with guidance from the counsellor, the client can forge new positive/adaptive associations with the targeted memory.Some highlights about this approach include:
Does not require talking in detail about the distressing issue or completing homework between sessions
Is designed to resolve unprocessed traumatic memories in the brain
Is applicable to wide variety of people and presenting problems (ie. Anxiety, panic, stress, trauma, just to name a few)
Can take less time to achieve symptom reduction compared to other therapeutic modalities
What is CBT-I?
Cognitive behavioural therapy for insomnia (CBT-I) aims to improve and change habits, thoughts, and behaviours that negatively affect an individual's sleep. It involves sleep restriction, stimulus control and relaxation practices. CBTI-I is a proven and effective treatment with 70-80% of clients showing improvement across several domains (sleep time, reduction in wakefulness and sleep onset) by end of the program.An important note is that a diagnosis of insomnia is not required to participate and to find benefit from the treatment program.Treatment is usually 6-8 sessions, but may vary depending on the client’s needs and presentation. Clients can expect working with the therapist to identify relevant targets for change and learning about sleep processes. Tasks such as completing a sleep diary will be expected outside of sessions.
What is CBT/BA?
Cognitive Behavioural Therapy (CBT) is an approach for a range of emotional health needs including depression and anxiety. It features an inside-out approach where the aim is to change the way you think in order to change the way you feel or behave. Features of this approach involve:
Recognizing and addressing maladaptive/unhelpful ways of thinking (automatic negative thoughts, cognitive distortions)
By recognizing problematic thoughts and shifting ways of thinking, it can help relieve the individual of problematic symptoms
Utilizing problem solving skills to promote feelings of self-efficacy
Behavioural Activation (BA) is an approach similar to CBT but fundamentally different, that has received empirical support to be just as efficacious in treating depression. Unlike CBT, BA utilizes an outside-in approach, where changing the way you behave will promote changing how you feel. Essentially, BA focuses on the link between behaviour and mood.Sometimes behaviours we implement and practice provide that short term alleviation of stress or anxiety, but when practiced over a longer period of time may serve to actually promote dysfunction or increase stress and anxiety.Think about this for an example, you skip completing some homework so you can get a good nights sleep. Now if that is a one-off, that is fine for most people and they will continue to function as they normally have. However, what happens when you regularly skip completing homework, and do poorly on the upcoming exam due to not being familiar with the concepts? This is a very simplistic and short-term example, but also portrays the general concept behind BA. At first it was to reduce stress, but now that behaviour is causing you more stress due to it being practiced over a longer period of time.
Crisis Support Contact Info
National Crisis centre
Unsure if you or a friend needs help? Having thoughts of suicide? call or text 988, Canada wide, 24 hours a day, 7 days a week, and get in touch with a responder who will listen, talk things over and do their best to give you support.BC Mental Health & Crisis Response
310-6789 (no number pre-fix ie. 604 or 778)
24 hours a day, 7 days a week.BC Suicide Prevention and Intervention Line
1-8001-800-SUICIDE / 1-800-784-2433
24 hours a day, 7 days a week.Kid’s help phone
For children and youth aged 5 to 20. Call 1-800-668-6868 to speak to a professional counsellor, 24 hours a day. It’s free, confidential, anonymous and available across Canada. They can also refer you to local services and resources.Immediate Risk
If you believe you or someone else is in immediate, life threatening danger, please call 911 or go to your nearest Emergency Room.Mental Health Information
Canadian Mental Health Association
Click the link for informative, downloadable pdfs about loss/loneliness/stress/anxiety/and various other topics.Here to Help BC
Host to a variety of self-help resources, information on common mental health challenges, and cursory self-screening tests.
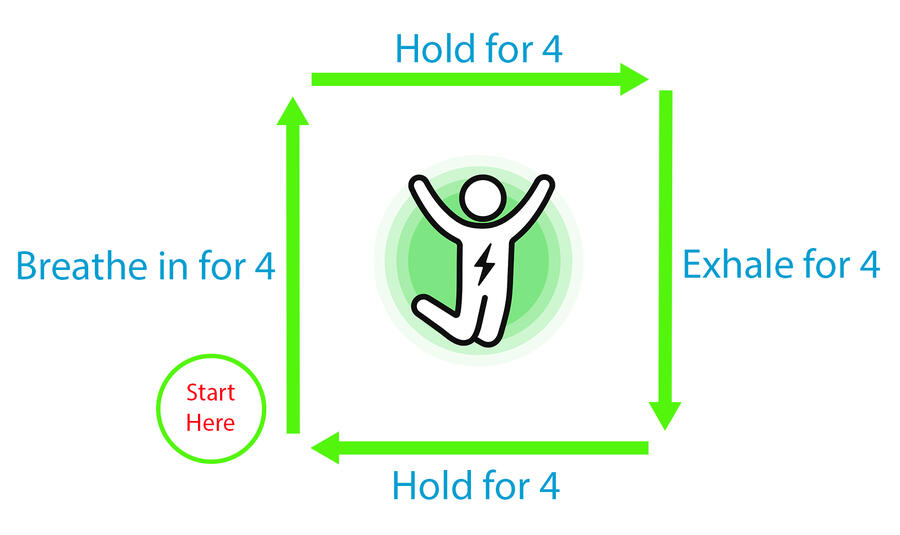
Mindful Practices
For everyday stresses, there are a multitude of techniques you can employ on a regular basis and we've listed a few of our favourites, some of which you may know already (possibly by a different name) or may be new to you.Hopefully you find one or two of these helpful!
Choosing a Counsellor
Choosing a Counsellor can be quite the intimidating task as the steps can be overwhelming with so many options or decisions to make. Here are a few tips that might help you make an informed decision about who to work with.
Shop around - Look through your local registry (ie. BCACC profiles) and use some keywords related to your concerns to narrow down your search (ie. Do they mention having experience in the field of your concern?)
Take caution if they list a high number of modalities as there is a difference between what a clinician may know theoretically and what a clinician actually practices/is trained to practice in. There is no set number, but after reading through profiles you will get a better sense.
Make a note of a few profiles that appeal to you or pique your curiosity and book some consultations (most offer a free consultation).
Come to consultations prepared with a brief description of your concerns as well as any questions you may have about the counsellor (ie. education, training, approach).
Review your consultation experience and think about if you felt like they were easy to talk to, understood your concerns, or gave satisfactory answers.
Don't be afraid to try working with a counsellor for a few sessions then changing professionals due to not feeling like they understand, or if you feel like the envrionment is not secure/safe for you to do the necessary work. (If this is the case, bringing it to your counsellors attention may be beneficial in changing their approach to better match your needs, but only if you feel comfortable to do so.)